Emergency contact: 01707 666399
Canine Cataracts

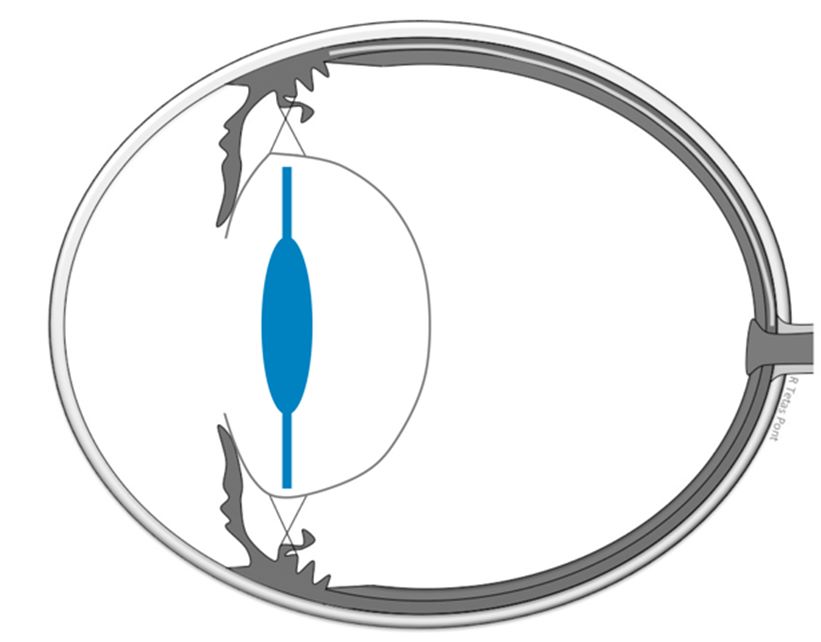
Cataracts are one of the most common causes of vision loss in dogs and frequently lead to blindness. In a healthy eye, light passes through the cornea (wind screen of the eye) and the lens to reach the back of the eye (retina). The lens is a transparent disc in normal conditions and is located behind the iris (coloured part of the eye). A healthy lens allows light to enter the eye and the lens focuses the light onto the retina producing a sharp image.
A cataract is where the lens becomes opaque (cloudy), interfering with the passage of light. A cataract may be a small speck that hardly interferes with vision or much more severe, leading to vision loss. Cataracts can also lead to loss of the eye if they remain untreated and deteriorate.
Vet Professionals: need to refer a patient?

What causes cataracts?
Most cataracts in dogs are the result of a genetic or hereditary defect. Many dog breeds are predisposed to hereditary cataracts, which may occur as early as at birth or develop later in young or middle-aged dogs. Dogs affected by hereditary cataracts should not be used for breeding.
Other causes of cataracts are diabetes, advanced age, trauma, or retinal disease. Depending on the cause, cataracts may or may not progress to total blindness. The degree of progression is often predictable and can be determined by means of a detailed examination by a specialist in veterinary ophthalmology.
How are cataracts treated?
The only effective vision-restoring treatment for cataracts is surgery, which is performed under general anaesthesia. Cataract surgery is usually performed with a technique called phacoemulsification. This technique uses special equipment to fragment and remove material inside the lens. The goal of the surgery is to remove the opacity and place an artificial intraocular lens (IOL) in the lens bag.
The vast majority, though not all eyes, can have an IOL placed, which will help the eye to focus light on the retina. If no IOL can be placed, your pet will be far-sighted but able to see.
To help the ocular health after surgery, all patients treated at the RVC are treated with daily eye drops for life.
Surgery is recommended in both eyes at the same time (bilateral surgery) if both eyes have operable cataracts. The recommendation is based partly on the patient requiring only one anaesthesia and post-operative period.

Is cataract surgery suitable for my pet?
Surgery is usually recommended when cataracts cause a significant visual deficit, when the cataract is progressing, and vision loss is predictable and/or when the presence of a cataract is likely to affect the health of the eyes for other reasons.
Prior to surgery, we need to determine if your pet’s eyes are healthy, apart from the cataracts – if they are ready to see again when the cataracts have been removed. Some pets have concurrent additional problems, such as dry eye, inflammation (uveitis), retinal degeneration, retinal detachment, or glaucoma (high pressure in the eye). These problems could make cataract surgery riskier.
A thorough examination, followed by some tests are routinely performed to detect these problems:
- Ocular ultrasound: will allow us to look into the eye behind the lens. This test is usually performed before the surgery under topical anaesthesia.
- Electroretinography (ERG): will allow us to check if the retina works. This test is usually performed under general anaesthesia just before the surgery.
- Other tests: blood tests and urine analysis may be required to assess if your pet is fit for the general anaesthesia.
How much does canine cataract surgery cost?
The cost of the surgery at the RVC is from £4100 (for one eye) and £5050 (for both eyes)
What is the success rate of cataract surgery?
Cataract surgery in small animal patients (dogs and cats) is considered a routine ophthalmic operation. The success rate is considered high, at approximately 90% - nine out of ten eyes have a favourable surgical outcome. The success may differ in each patient. The success rate is higher in cataracts that have appeared relatively recently than those that are months or years old.
Concurrent ocular problems to the cataracts can make the surgery less successful. After the full examination, we will indicate the risks and benefits of surgery and help you to make the best decision for your pet.
What are the risks and complications of cataract surgery?
There are inherent risks to any ocular surgical procedure and to general anaesthesia. Cataract surgeons at the RVC are trained specialists, working with specialist anaesthetists.
Complications may include:
- Post-operative hypertension (POH)
- Intraocular inflammation (uveitis)
- Lens fibre regrowth
- Glaucoma
- Retinal detachment.
Given the high success rate, complications are considered low (one in every ten animals is expected to suffer from a particular complication). The most common are inflammation and lens fibre regrowth. The most serious are glaucoma and retinal detachment. Complications can increase over time, thus it is very important that an ophthalmologist examines your pet at least once every 9 to 12 months after surgery, for life. Complications occurring in both eyes are uncommon.
- Post-operative hypertention (POH)
POH occurs when the pressure in the eye is elevated after surgery. Although POH is usually short lasting, self-limiting and carries a good prognosis, it requires treatment with drops. At the RVC we hospitalise animals overnight after surgery to look for POH.
- Inflammation (uveitis)
All cataracts cause uveitis, and this may persist after surgery. Diabetic dogs have more pronounced uveitis. Long-term uveitis can lead to serious problems like glaucoma or retinal detachment. Control with medical therapy (drops) if possible. Some cases might require a surgical intervention. Long term follow-up of all patients is vital to help control uveitis.
- Lens fibre regrowth
This occurs when the lens forming cells grow after surgery. This happens more rapidly in young patients undergoing surgery. This complication rarely interferes with vision but may require surgery if very severe.
- Glaucoma
A long lasting and serious problem that is associated with a persistently elevated pressure in the eye leading to blindness. Medical and surgical treatments exist but glaucoma carries poor prognoses for sight in the long term.
- Retinal detachment
The retina can become detached from the back of the eye, partially or completely. A total retinal detachment causes vision loss. Some retinal detachments may be treated with surgery or laser treatment in dogs.
Aftercare
Aftercare is the most important part of the post-surgical recovery period as it can affect the long-term prognosis. Patients undergoing cataract surgery routinely spend two nights in hospital – the night before and the night after surgery. They are discharged from the hospital with a set of instructions.
- Protection: All animals have to wear a protective collar for two weeks after surgery to shield their eyes from accidental trauma. It is vital that the collar is not removed for the length of this period. Eating and drinking can be tricky with the supplied collars, but smaller collars do not protect the eye. You can help by elevating food or water.
- Exercise and activity: Should be restricted to prevent eye injuries. Short, relaxed walks are allowed on a short lead, and with the collar on at all times for two weeks after surgery. In week three and four after surgery, walks can be a bit longer but still on the lead. It is very important that dogs no longer play “tug-of-war” or “hunt and shake” with make-believe prey objects, as head shaking can harm the eye. Many dogs will love to play these games but the good news is that dogs quickly take to fetch and other interactive games that also involve owners. The use of a harness is always recommended in patients that undergo eye surgery as pulling on the collar increases the pressure in the eye.
- Medication: Eye drop(s) are administered in a tapering application regime, starting at 4 to 6 times daily. This is usually reduced over 3 to 4 weeks to once or twice daily, depending on the ocular health of each individual patient. Oral medication is also given for about three weeks after the surgery.
- Examination at the RVC: Re-examinations are vital to assess ocular health over time and to avoid complications. Usually, a re-examination is required one week after surgery, then three weeks after, three months later and then six months later before seeing the patient once every nine to twelve months for life. This schedule will be adapted to suit the individual needs of each patient. Re-examination costs are not included in the surgery estimate.
If no severe complications, vision is recovered immediately after the surgery. However, in most animals the vision improves slowly over the first few days after surgery. Eyes are normally red with mucoid discharge in the first few days after surgery. Sometimes the eyes “look tired” and may look a little sore or light sensitive over the first few days.
Out of hours, the RVC operates an emergency service that you may contact if you are concerned after surgery. This service operates as any other emergency service, including the payment of an emergency fee that is not covered in the estimate for surgery. The RVC emergency service has access to an RVC ophthalmologist if required.

